If you grew up in Arizona or California — or you’re obsessed with the HBO series “The Last of Us” — you may already be familiar with the dangers of fungal infections, particularly Valley fever. And while the vast majority of Valley fever cases are reported in the Southwest, experts are saying the fungal infection is spreading due to climate change.
The Centers for Disease Control and Prevention reported roughly 20,000 cases of Valley fever in 2019, with the caveat that this number is likely underreported by tens of thousands due to misdiagnosis. In the same year, a study tracking Valley fever predicted the number of cases could “more than double” by the year 2100 and expand north into drier states in a “high warming scenario.”
Valley fever used to be referred to as “desert rheumatism” because of its correlation to the desert climate and its impact on the lungs, according to the University of Arizona. The fungus that causes the respiratory illness is found in hot, dry environments, which is why as the planet heats up, experts have predicted Valley fever will expand past the Southwest region. “In general, different fungal species have different environmental conditions that allow them to flourish,” says Amesh A. Adalja, MD, FIDSA, FACP, FACEP, senior scholar at Johns Hopkins Center for Health Security. As environmental conditions change, more areas may become hospitable to their growth.
But is this cause for concern? “Valley fever isn’t particularly dangerous to someone with an intact immune system,” Dr. Adalja explains. “However, in the immunocompromised, Valley fever can be very dangerous and can disseminate throughout the body and cause very severe infection.” Not to mention, long COVID and certain treatments for cancer and other diseases have created a more immunosuppressed population, says George Thompson, MD, professor of clinical medicine at the University of California, which can make people more susceptible to fungal infections like Valley fever.
POPSUGAR spoke with health experts about everything you need to know about Valley fever, including symptoms to watch for and how to treat an exposure to the sometimes-deadly fungal spores.
What Is Valley Fever?
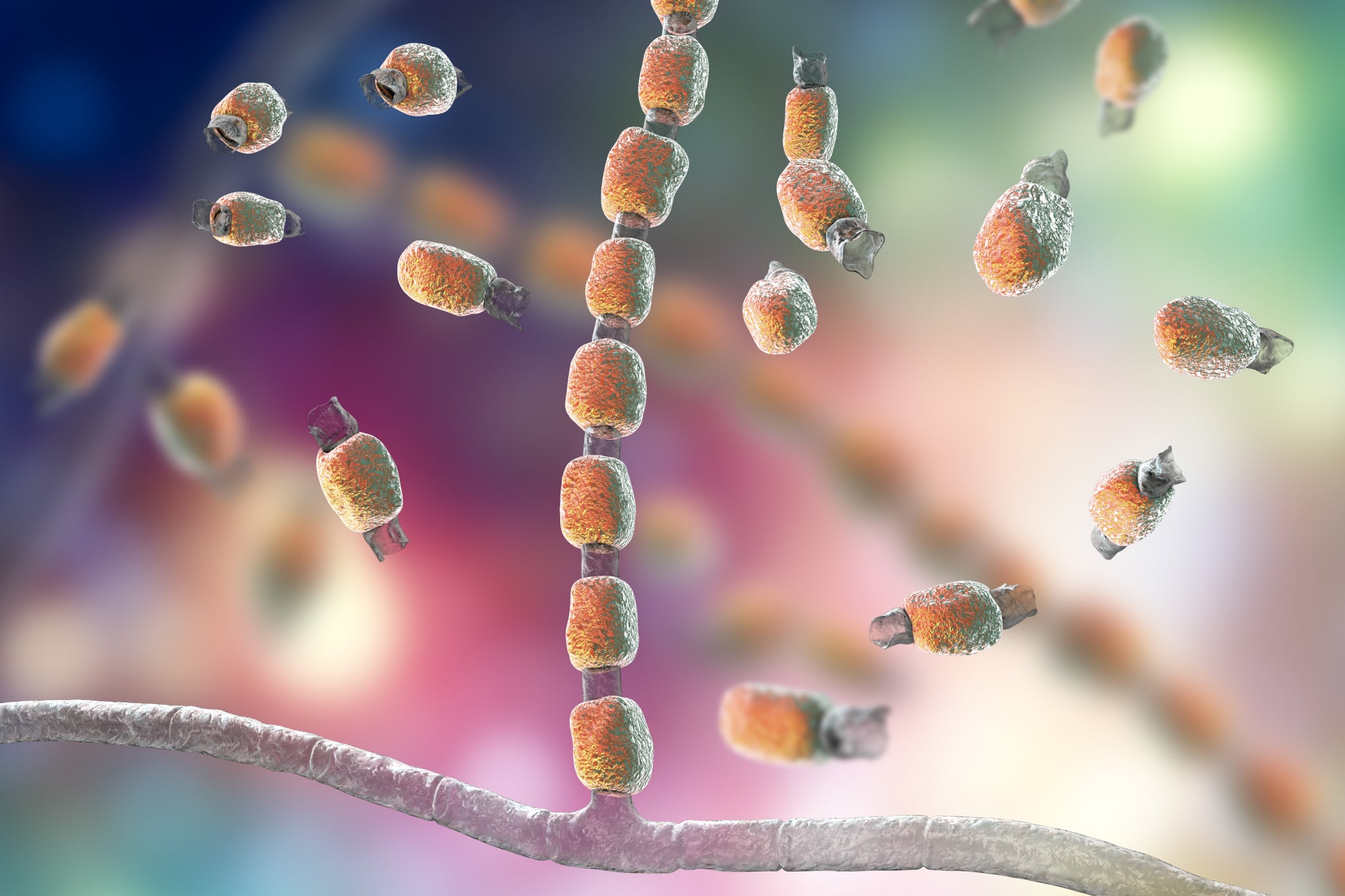
Valley fever is a lung disease commonly found in the Southwest because it thrives in areas with low rainfall, high summer temperatures, and moderate winter weather. It’s also known as coccidioidomycosis or cocci because it’s caused by the fungus Coccidioid that grows in soil. The respiratory illness can be deadly, especially for the immunocompromised and domestic animals. Take steps to prevent fungal infections, such as wearing protective clothing when working in areas with a high risk of exposure and being mindful of the symptoms.
Valley Fever Symptoms
Symptoms are typically mild and flu-like and occur within three weeks of exposure. “In some cases, the infection may also cause joint pain, skin lesions, and rashes,” says John Landry, registered respiratory therapist and CEO of Respiratory Therapy Zone. “If left untreated, Valley fever can spread to other parts of the body, such as the bones, causing more severe symptoms, including bone pain, joint swelling, and inflammation.”
The most common symptoms, according to Cleveland Clinic, include:
- Persistent cough
- Chest pain
- Fatigue
- Fever
- Headaches
- Rash
- Night sweats
- Joint or muscle aches
It is important to note that not all individuals with Valley fever will experience symptoms, and some may only experience mild symptoms that resolve on their own. “However, it is still important to seek prompt medical attention if you believe you may have contracted the infection, as early treatment is key to managing symptoms and preventing complications,” Landry adds.
Is Valley Fever Contagious?
Valley fever isn’t a contagious disease, per the CDC. Infection occurs when a fungal spore is inhaled. The spores become airborne when the soil is carried in dust particles by the wind.
How to Test For Valley Fever
To diagnose Valley fever, a healthcare provider will typically order a blood test to detect antibodies or antigens to the fungal spores, explains Oladele Ogunseitan, PhD, MPH, University of California presidential chair, professor of population health and disease prevention. “Microscopic analysis of tissue biopsy and culturing (growing) of the fungus from tissue samples can confirm infection,” he adds. “And chest X-rays or CT scans of lungs can also detect pneumonia due to Valley fever.”
Valley Fever Treatment
Treatment for Valley fever can vary depending on the severity of the infection. In mild cases, at least 95 percent of patients with the fever fully recovered without treatment, according to the Valley Fever Center for Excellence (VFCE). In more severe cases, antifungal medication may be prescribed to help clear the infection. The “azole” family of antifungal drugs (commonly fluconazole or itraconazole) are frequently used to contain the fungus from spreading outside of the lungs but can’t kill it, per VFCE.
In some cases, where the infection has spread to other parts of the body, such as the bones, surgery may be necessary to remove the infected tissue. “Treatment for Valley fever can be a long and challenging process, often requiring months or even years of medication and close monitoring by a healthcare provider,” Landry says. “However, with proper treatment and care, many patients are able to make a full recovery.”
The VFCE, along with a California-based biotech company and Colorado State University, are developing a vaccine to combat Valley fever. According to the center, they are in the early stages of drug testing, but there is currently no cure.